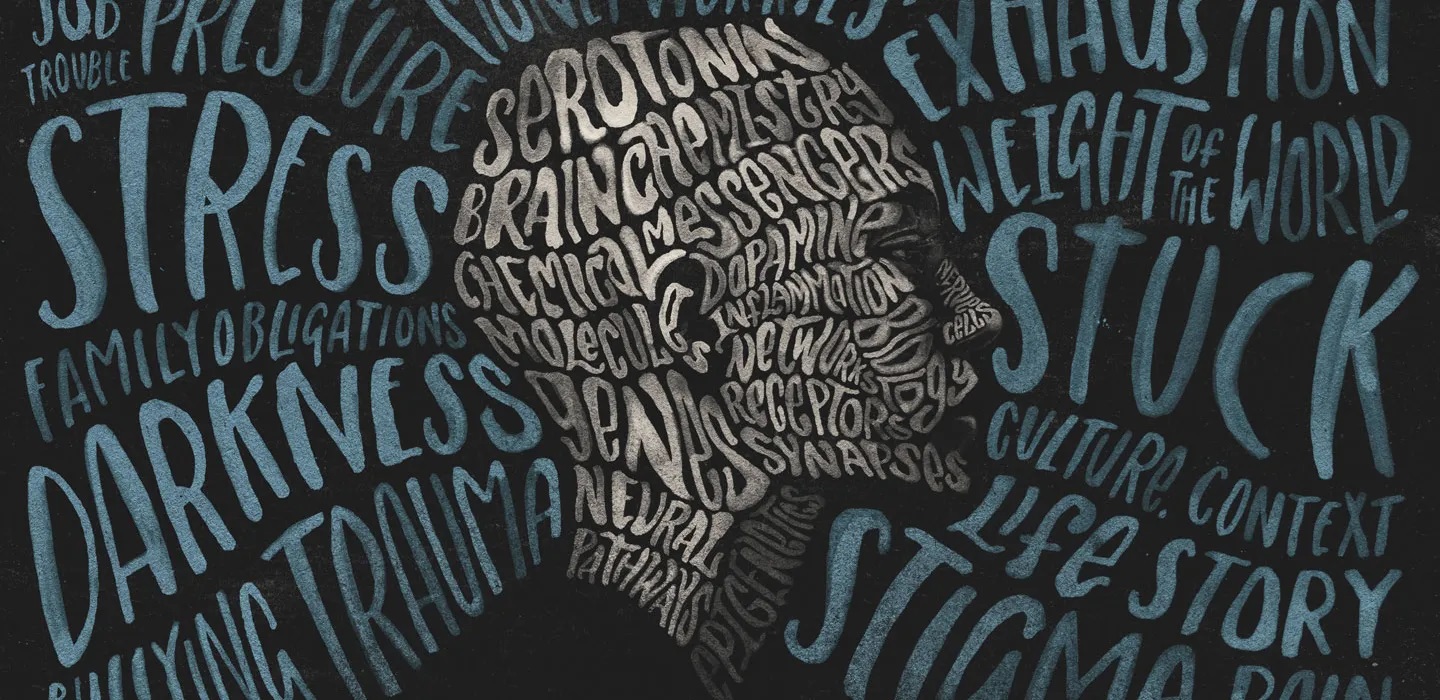
(Photo : Depression)
Depression
- Depression has been linked to inflammation, with stress activating inflammatory processes in the brain.
- Research by Professor Raz Yirmiya has identified potential therapeutic targets, suggesting personalized treatments based on individual inflammatory profiles.
- Traditional depression treatments often fail to fully explain why some people respond while others do not, leading researchers to explore the role of inflammation.
- The research underscores the importance of a holistic approach to mental health treatment, considering both psychological and physiological aspects.
Depression, a prevalent mental health disorder, has been linked to inflammation in groundbreaking research. Neuroscientist Professor Raz Yirmiya from the Hebrew University of Jerusalem has made significant strides in understanding the role of microglia cells and interleukin-1 in stress-induced depression.
His research suggests that exposure to stress, a significant trigger of depression in humans and animals, activates inflammatory processes, particularly in the brain. This revelation fundamentally alters our understanding of the biological underpinnings of depression.
Yirmiya's team employed a combination of molecular techniques and behavioural studies to identify several promising therapeutic targets. Their work on microglial checkpoint mechanisms and stress resilience has opened new avenues for understanding how the immune system influences mental health.
These findings suggest the potential for developing personalised treatments based on individual inflammatory profiles. Yirmiya's work indicates that both activation and suppression of the immune system can trigger depressive symptoms. This highlights the need for personalised treatment approaches that take into account the unique inflammatory profiles of individuals.
Exploring New Angles in Depression Treatment
In addition to the primary source of information, several other relevant news sources provide further insights into the link between inflammation and depression. For instance, a study on stress-related brain inflammation linked to depression revealed that traditional treatments primarily focused on correcting imbalances in neurotransmitters like serotonin, dopamine, and norepinephrine.
However, these traditional perspectives often fail to fully explain why some people respond to treatments while others do not. These limitations have driven researchers to explore new angles, such as the role of inflammation, to uncover hidden contributors to the condition.
Another study on transcriptomic profiles in major depressive disorder highlighted the role of immunometabolic and cell-cycle-related pathways in depression with different levels of inflammation. The study found that most of the pathways differentiating between different levels of inflammation in major depressive disorder share common molecular mechanisms, enriched in genes involved in the organism's defence and immune response.
The Role of Corticotropin Releasing Factor in Depression
A study on the role of Corticotropin Releasing Factor in the Neuroimmune Mechanisms of Depression suggested that Corticotropin-releasing factor is a key component of the hypothalamic-pituitary-adrenal axis, a major regulator of endocrine stress response.
Different brain regions are involved in the stress response system, such as the amygdala, hippocampus and the prefrontal cortex. During the stress state, the neuronal activation in these regions converges on the hypothalamus and activates the endocrine stress response.
The new understanding of depression's biological underpinnings could lead to more targeted and personalised treatments. However, more research is needed to fully understand the complex interplay between the immune system, inflammation, and mental health.
The findings underscore the importance of a holistic approach to mental health treatment, taking into account not just the psychological, but also the physiological aspects of the condition.









